As mentioned in previous posts, during my surgery the plastic surgeon placed two tissue expanders under my chest muscle to replace the breast tissue removed by the breast surgeon. In case you don’t know what a tissue expander is (I didn’t), it’s basically just a temporary, inflatable breast implant designed to stretch the skin and muscle to make room for a future, more permanent implant. (See images below.) Each of the expanders includes a port through which a saline solution is injected during fill appointments (thereby enlarging the expanders).
This past Thursday–roughly 2 and a half weeks after my surgery–I went in for my first fill appointment. I wasn’t too nervous as I had done a lot of research on my own and based on conversations with other women who have had this, it really shouldn’t hurt. If anything, I was actually kind of excited as it meant that my body had healed a decent amount and getting the expanders filled would be kind of fun (in my mind). To begin the appointment, the PA removed the steri-strips from both scars on my chest, which were still pretty raw. She then took out a magnet to find the location of each expander’s port and marked the location on my skin. She then inserted a needle through my skin at the marked location and, with a syringe, injected 60 CCs of saline into each expander. (As mentioned in an earlier post, only a fraction of the total volume is injected during each fill appointment to allow the skin and muscles to slowly stretch.)
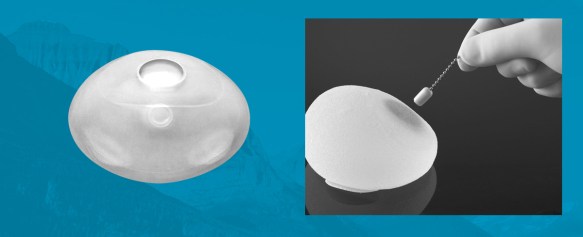
Left: an expander; Right: example of the port’s magnetic properties [Image courtesy of Specialty Surgical Products, Inc.]
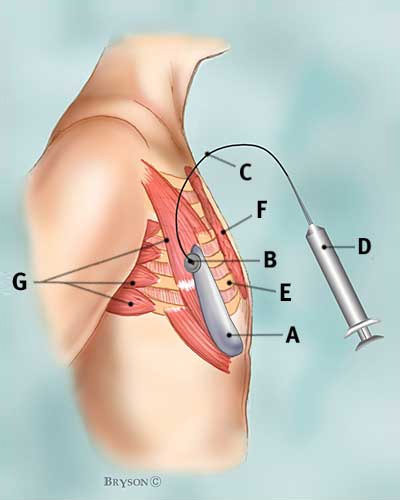
[Image courtesy of breastcancer.org]
A Tissue expander — unfilled
B Port
C Catheter
D Syringe
E Ribs
F Pectoralis major muscle
G Other muscles of the chest wall
Because I now have permanent loss of feeling in the chest area, the injections didn’t hurt at all (a nice perk). The PA warned me, however, that I may have pain and discomfort later in the day or the next morning. Unfortunately, she was right. About three hours after the appointment, I began experiencing moderate pain in my chest which lasted for about a day. It wasn’t debilitating but noticeable enough that I barely slept that night (no longer on narcotics, just rotating Advil/Tylenol) and didn’t want to move much.
The plan is for me to continue with fill appointments on a weekly basis (with the exception of this week – Happy Turkey Day!) until I reach my desired size. At that point I can schedule my final surgery which will be, at the earliest, early February. One month before my final surgery, I have an additional fill appointment where the expanders are enlarged beyond my desired size to allow more room for Dr. Fine to work with during the final implant surgery.
One of the first questions I have received from oh, a strong 80% of people that I’ve spoken with about my surgery was, “So you getting bombs?” The quick and short answer is NO; I wouldn’t know what to do with them and would likely topple over (but still an entertaining thought…I think my family would die). After a few laughs and a “but really, just imagine it, hilarious” the question evolves into, “But seriously, what size and how do you decide?”
The doctor can’t tell you that X number of fill appointments will make you a B or C cup (or beyond, get it girl), as it completely varies based on the frame of the individual. What the PA and one of the women I spoke with recommended was to either: (1) buy a bra the size you want to be and continue with the fill appointments until the bra fits correctly or (2) continue the fill appointments until your clothes get to a point that they almost no longer fit. As I was happy with my body and chest size prior to the surgery, I plan to do a combo of 1 and 2. I don’t want to go to a point where I would have to order clothes a size up to fit my chest but then would need to get them tailored down to fit my body. I also don’t want to look all that different. BUT – the option is always there for any woman that goes through this. I say: if you want it, get it. If you get it, flaunt it. You’ve put your body through some shit, so if you decide to “go big or go home” then by all means do, who is anyone to judge.













