I know this post may come as a surprise to most people, as T wasn’t scheduled for her final surgery until Friday, February 12th. But she started having some issues earlier this week, and had her surgery yesterday mid morning!
Wednesday morning started out as a normal day. T went to the gym early before work. When she got out of the shower (at the gym), she noticed some blood on her towel, and thought that her nose was bleeding. She checked her nose and realized it wasn’t the source of the bleed, and after a few seconds of checking around, it became apparent that the bleeding was coming from the edge of her right incision. There was a dime size, circular area that had developed, was very red, and was bleeding (see a “zoomed in” look of her incision swelling below).

Unable to take a picture of the area, T nicely asked a random woman in the locker room if she could take it for her. T explained to the woman her situation (prior to asking her to take the pic for her), and it just so happens that this woman’s father was recently diagnosed with breast cancer. T and this woman had a short, but intimate conversation about this, BRCA2, and the Bright Pink Organization (which she encourage T to look into) and I think it is testimony to the saying that everything happens for a reason (as Cheryl would most definitely say!). This nice woman took a picture of the swelling area for T, and she sent it to her nurse immediately.
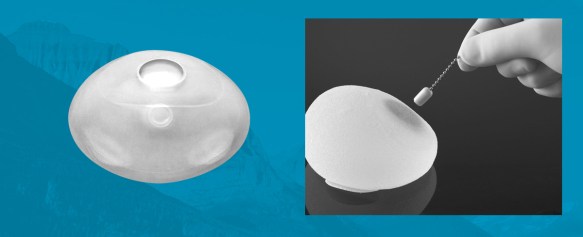
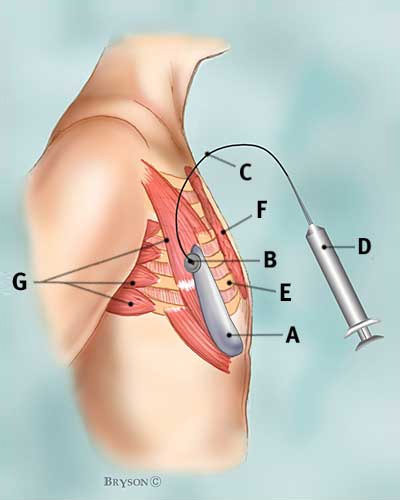
Upon receiving the picture, and the nurse called and asked T to come in as soon as possible to meet with Dr. Fine. Because Dr. Fine was tied up in surgery, T saw one of his partner’s P.A.s, who immediately wanted one of the docs to see it. They brought in a different physician, who drained 60 cc of saline from the right expander. He covered the incision with 2 steri strips, and then told T that she needed to to push up her surgery to as soon as possible and he would go speak with scheduling and inform Dr. Fine later that morning. The physician was concerned that the incision opening would not make it until her February 12th surgery date (basically that it would continue to open, the expander would become exposed, infection can start/expand). Luckily, Dr. Fine had an opening on Thursday AM and they just need to secure an OR spot and anesthesiologist.
We were all shocked and worried when T sent out a group message to our family (yes, our family has a daily “whatsapp” group message going) to let us know that she would be going in for surgery not next week, but tomorrow (Thursday 2/4/16). I called T to discuss this with her, and I so impressed and proud of her for being so brave. She no longer had another full week to mentally prepare for her surgery – she now had less than 24 hours. I can’t even imagine what would be going through my mind if I were in her shoes. When T is further along in the recovery, I know she will post and she can express her thought process throughout all of this craziness! But from my perspective on the other end of the phone, she was as cool as a cucumber – she got everything taken care of with work and was ready to go! My mom, being the wonderful mom she is, immediately packed her belongings and drove to Chicago on Wednesday night. She arrived to T’s apartment around 8:30 pm.
Her surgery was slotted for 10:30 AM on Thursday morning, February 4th. T and my mom woke up, had breakfast (Cheryl), read the paper, and then headed to the hospital around 8:30 AM. When I spoke to T yesterday morning on the phone, she sounded relaxed and ready for the surgery. If she was scared, I sure couldn’t tell. We chatted for a few minutes – I told her that I felt that even though this surgery was sooner than she expected, the suddenness of everything wouldn’t allow her any extra time to worry or over-analyze her thoughts for another week. She was finally at the last “pit stop” of this journey, and she was so close to the finish!! I respect and look up to T so much for being so brave, so light hearted, and so open minded throughout this whole process. I know that I could not have handled all of this so gracefully!
T’s surgery didn’t actually begin until closer to 11:45 AM. Dr. Fine was held up in a previous surgery, where his patient’s expander edge broke through her skin, which is the concern the doctor had for T’s prior issue which resulted in her getting a second over expansion. Once the surgery began, it lasted for about 2 hours. My mom did a great job keeping us all posted via calls and texts. When T got to the recovery room, her core temperature was only 95 degrees, so they had to use a machine to help increase her body temperature to normal. While it didn’t seem “normal” to T at the time, apparently this does happen quite frequently for these types of surgeries, where the patient is lying for quite some time with their chest cavity open, in a cold surgical room.
After a few hours in the recovery room (and once her body temp was back to normal), T was able to head home with my mom. She got home around 4:30 pm, where she returned to her previous post-surgery spot: the couch!

T was in quite some pain yesterday afternoon/last night upon arriving home. She is taking Norco (q 4 hours) and Tylenol in between as needed. The pain is much greater this go around in comparison to her previous surgery. Last time, she had a local anesthetic pump “built in” that delivered local anesthesia as needed, in addition to her pain medicine regimen. She also had a larger surface area numbed for the last surgery, in comparison to this one, which took longer to wear off. She again has a scopolamine patch behind her ear, which will stay there for three days to help with nausea. T was able to eat some food last night, mainly soup, a few graham crackers, nuts, and an orange. I got to speak with her around 8:45 pm (central time). She expressed that she was in pain, but at the same time she was in good spirits, and very happy to have reached this point in the process.
I know T is in the best of hands (thanks to Cheryl) as she attempts to get a good night’s sleep on night #1 post-surgery. I can’t think of anyone more comforting at a time like this than Cheryl….. #numberonemom.
Sleep tight T!!!! (hopefully!)